Updated Nursing Facility Report
Dr. Charlene Harrington (and colleagues), from University of California San Francisco School of Nursing, have updated the report, “Nursing Facilities, Staffing, Residents and Facility Deficiencies, 2009 Through 2016,” over the previous version that included data through 2015. (available here: Harrington 2009-2016 )The report offers summary information from OSCAR (On-line Survey, Certification, and Reporting system)/CASPER (Certification Survey Provider Enhanced Reports) data. The previous version of the report was published in 2017 (previous version here: Report).
OSCAR data is a national compilation of the information gathered by surveyors during nursing facility inspections occurring at least every 15-months and required for participation in Medicare and Medicaid programs. It contains information on nursing home operations, census, and regulatory compliance. It is aggregated by the Centers for Medicare & Medicaid Services (CMS) in cooperation with long-term care surveying agencies in each state. The original OSCAR system was converted to what is now known as CASPER in 2012.
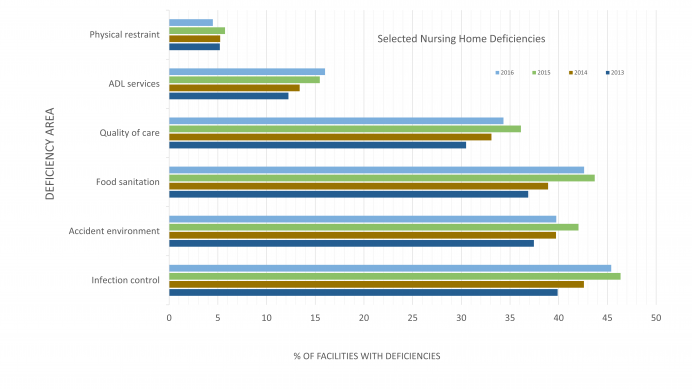
Dr. Harrington’s report summarizes a variety of metrics about nursing homes, their residents, staffing, and care deficiencies, by state and year. The care deficiency areas, care areas that are found to be below established standards during a routine survey, are especially interesting, as the deficiency rate trends over multiple years can highlight areas that have gotten extra attention, or how waning attention has changed practices. These deficiency areas, such as physical restraints and tube feedings, are associated with poor patient outcomes.
The most common failures for which facilities were cited were in the areas of infection control, food sanitation, accident environment, and quality of care, among others. Overall, nursing facility deficiency rates have declined, but there is wide variation between the states. The use of physical restraints appears to be at a low of 4.5%, down from 10.8% in 2009. Interestingly, deficiencies in Activities of Daily Living Services (F312) increased each year since 2013, to its current rate of 16%.
Infection control is an area consistently in the top 5 for deficiencies. This standard states that “the facility must establish and maintain an infection control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of disease and infection.” Some 45% of facilities received a citation for infection control in 2016. This requirement includes many different care aspects, from handwashing procedures and vaccination to medication handling and infection control policies and training. With a big focus on C. difficile and drug resistant organisms, infection control should be a critical area for focus and education. Additionally, CMS finalized a new rule that went into effect November 2017, requiring the facilities establish an infection prevention and control program that includes antibiotic use protocols and a system to monitor antibiotic use. (F881)
The CDC and AHRQ has several resources on antibiotic stewardship for nursing homes that can be found here or here.